They tell you not to drink too much caffeine when you're pregnant. One cup a day is OK, but if you can avoid it, that's recommended. No alcohol, no smoking, and definitely no illicit drugs. You're not really supposed to share the news of your new pregnancy with the world until you're at least 12 weeks, which is considered the "safe zone." Sure, share with family and close friends, but Facebook doesn't get to find out until much later. Check, check, check.
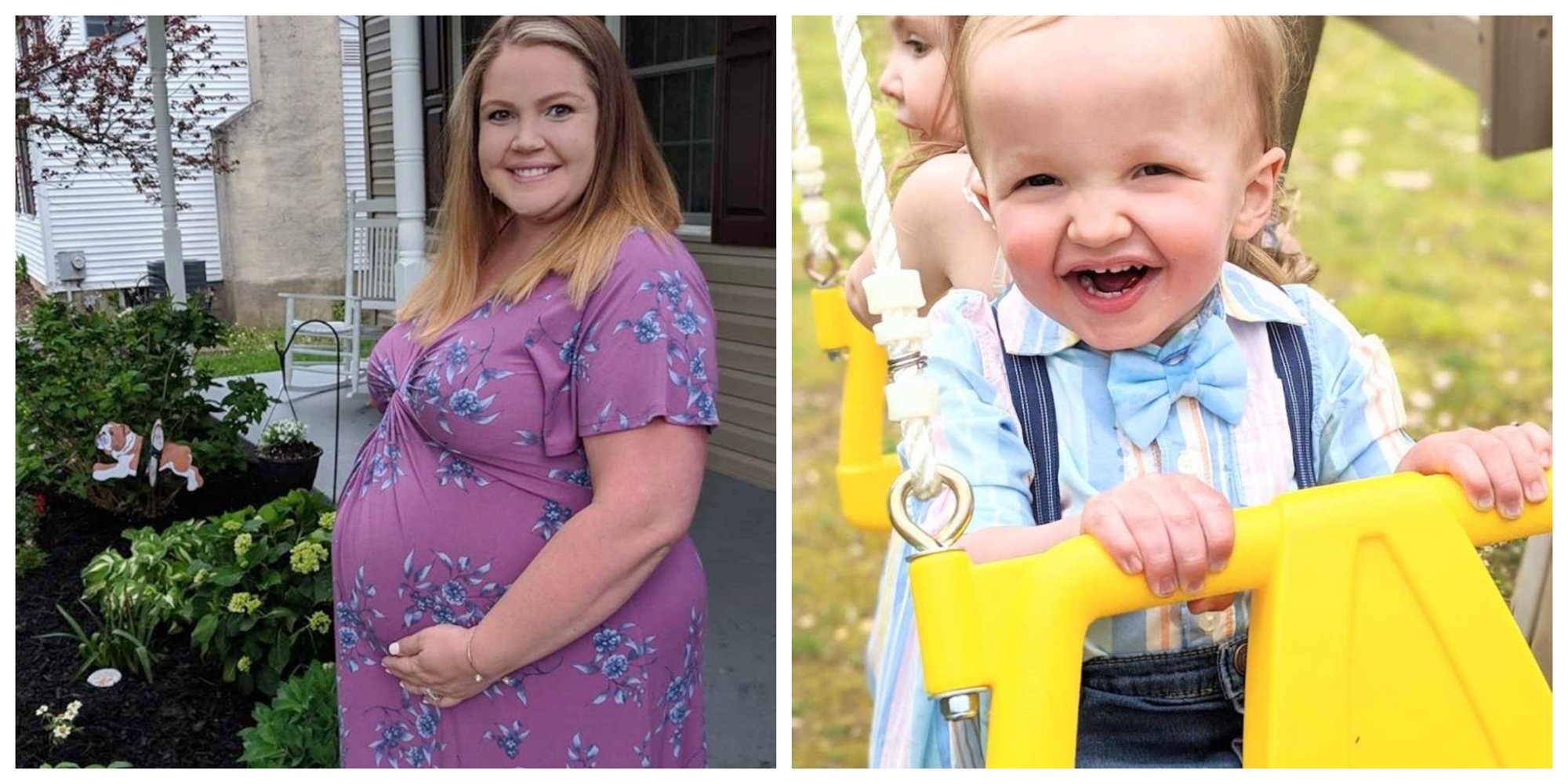
I followed the rules. I was 12 weeks along and thought I did everything right…

Our poor ultrasound tech showed up for work expecting a normal day and instead found herself scanning me, the mom carrying a potentially very sick baby. She and our doctor told us they saw excess fluid on the back of our baby's neck, which could mean a few things, namely life-threatening trisomies. I had to wait a week before we could scan again to confirm the fluid. A WEEK. Seven days. 168 hours. Do you realize how long that is for a worrying mother-to-be? You might as well have told me I was miscarrying because inside, I felt like we were both dying.
After some initial tests, our doctors couldn't give us straight answers.

We ended up undergoing invasive testing to determine what exactly we were up against. We saw geneticists and spent hours going over our medical histories in depth. We spent six long weeks waiting to hear good news, bad news, ANY news regarding the health of our baby.
Finally, at 19 weeks gestation, I got the call from our geneticist.
She said our baby BOY was utterly perfect. I cried. I laughed. I screamed so loud I sent the dogs running into the other room. We were having a healthy baby and a boy to boot! Oh, the relief…
It's ironic that mere days after receiving that incredible phone call, we found out about Jax's congenital diaphragmatic hernia diagnosis at our 20-week anatomy scan.
Completely unrelated to the first five months of unknowns, we were given a totally different, separate diagnosis to swallow.
(Read that again. Completely unrelated… what are the chances?!) Thinking back to that phone call makes me laugh, but the kind of laugh that chokes you and turns to uncontrollable tears because we dared to have hope.
At just over five months pregnant, we learned our sweet Jackson, the feisty, tumbling baby in my belly, did not have any trisomies but instead had a life-threatening birth defect known as a congenital diaphragmatic hernia.
CDH occurs as often as cystic fibrosis and spina bifida.

Ninety-nine of those people will have never heard of it and the one who "knows" what it is will likely only have secondhand experience. A congenital diaphragmatic hernia is when the baby's diaphragm fails to fully form, which leaves a hole, allowing organs meant to stay in the belly (liver, stomach, bowels, etc.) to migrate into the chest, where only the heart and lungs should be, compressing those organs and preventing growth. Out of 4 million babies born every year in the US, only 1,600 will be born with CDH, but out of those 1,600, only 800 will survive. 50%. Half. That's it.
When we first received Jax's diagnosis, we met with dozens of doctors, social workers, surgeons, specialists -- you name it.
All of whom looked at us like we'd already lost our child. While I'm sure they had the best intentions, the statistics they gave us didn't give us hope. They were preparing us for the burial we'd most likely be planning. Our surgeon told us if Jax survived, and his chances were not good, we would not take a deep breath for at least the first two years of his life. A NICU nurse bluntly asked us why we were having a baby shower for a baby that would most likely not make it.
Our maternal-fetal medicine doctor asked if we'd like to terminate.

Not only were we up against a devastating diagnosis, but we were also up against seasoned doctors who questioned our decision to give our son a chance at life.
After the scariest nine months of my life, I waited in a hospital bed at one of the best children's hospitals in the world, ready to deliver my baby boy. With my daughter, I couldn't wait to hear her first cry. I longed for our first moments of skin-to-skin, kissing her sweet, round head. With Jax, I lay on that operating table praying he would not cry. I begged him to be strong and brave and silent, for a crying baby with bad lungs introduces unwanted air (odd, I know, but true). While we were primed for how our birth would go, it could never prepare me for it in real-time. When Jax was pulled from my stomach, he didn't cry (yay!).
While still connected to me via the umbilical cord, he was immediately intubated. We didn't see his face. We didn't hear, "It's a boy!" My husband didn't get to cut the cord or place our new baby in my arms. Instead, Jax was taken to an adjacent room for 45 minutes so he could be prepped for his walk down to the NICU. As I was receiving my final stitches, they wheeled Jax past us and out the door. All I can remember is watching the nurse methodically pump a bag, effectively breathing life into my son, one squeeze at a time.
Five hours after giving birth, my husband and I were finally given the go-ahead to go meet our son.
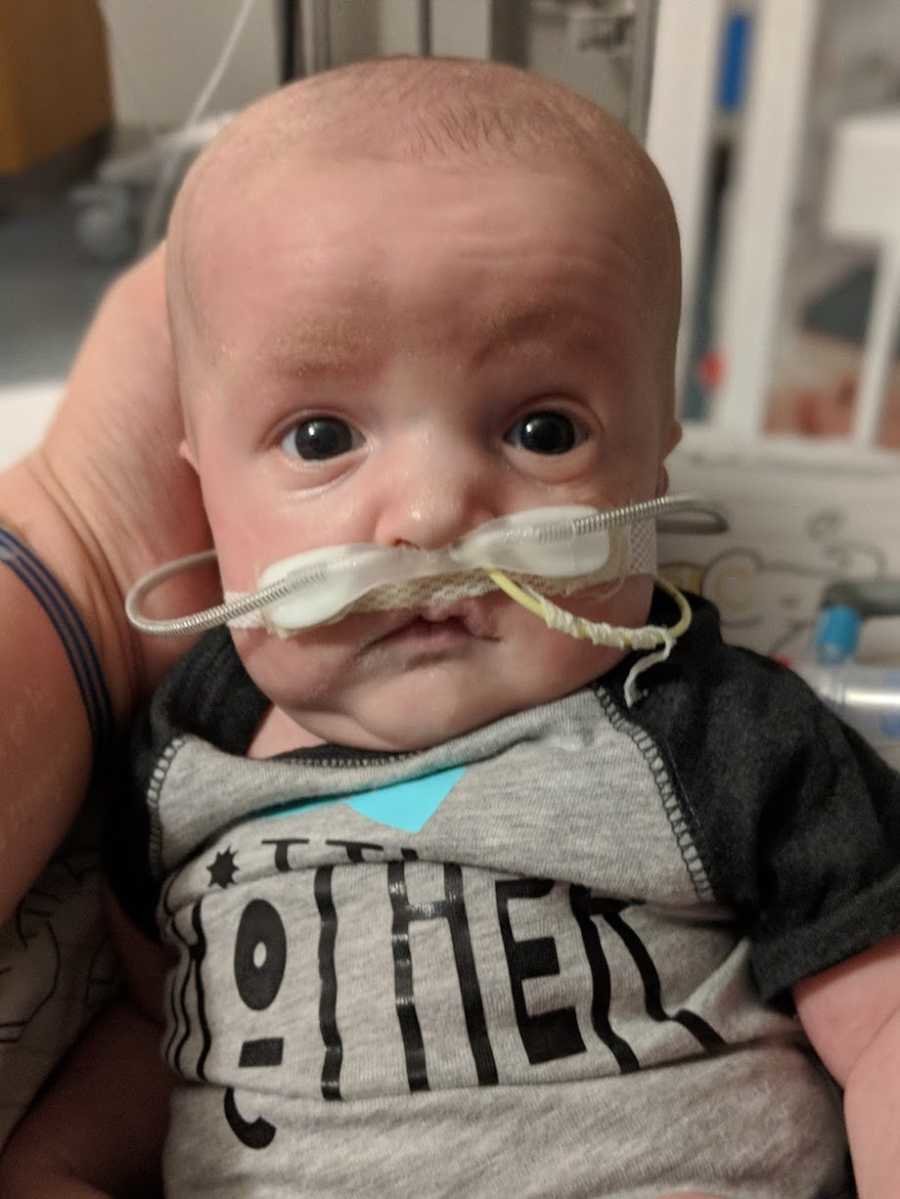
We trekked across the hospital and down to the NICU where no less than 15 doctors, nurses, and ultrasound techs surrounded our baby's bedside. Jax was receiving an ECHO (an ultrasound of the heart) to determine his stability. He was attached to cords, wires, tubes, you name it. I took one look at him from across the room and vomited. It was the most visceral reaction I've ever had to anything in my entire life. Seeing my hours-old baby hooked to machines keeping him alive was too much to bear.
We quickly realized our presence, while welcome, was an added pressure so we retired to our room.

About six hours later, our room phone rang and then my cellphone, neither of which I could reach or get to given my recent surgery (and my husband was snoring too loud to hear it himself). Our nurse came to us then, saying my husband was needed in the NICU immediately. Not me. Just my husband. Was something wrong with Jax? Wouldn't they also summon me, though? The next 20 minutes waiting for Matt to return were torturous and when he finally did, it was no easier hearing what he had to say. He told me: "The doctors just asked me to sign consent forms to put Jax on ECMO. They said to me, 'We need your permission to do whatever it takes to save your son's life.'"
Sucker punch. That's what it felt like, hearing those words.

Again, we knew the potential for ECMO was there given the severity of Jax's case, but knowing our son was actually being put on heart and lung bypass was devastating. At 12 hours old, our son was on life support.
The next 13 days were some of the hardest in our lives.

Daily, we'd make our way to his bedside, careful not to disturb the two huge cannulas attached to his neck, circulating blood through a machine and into his tiny body. We'd watch as our heavily sedated son desperately tried to connect with us by opening his eyes or ever-so-slightly moving a finger. We likely drove the nurses crazy, asking about every beep, every number, and Jax's chances at survival. Not big on prayer, we relied on science and data to keep us from drowning in fear and sorrow.
On May 31, 2018, Jax's due date, we got the news Jax was strong enough to come off ECMO.

He'd faced a couple of infection scares and needed a complete ECMO circuit change at one point. Thirteen days of life support later, Jax was proving he might be able to handle it. To be honest, by that point, we'd become accustomed to the ECMO machine and the security it provided our boy. We were definitely a little nervous to leave that blanket of protection behind, but as we'd soon learn to be Jax's style, he completely crushed it.
Two weeks later, Jax underwent his third and most important surgery: CDH repair.

At just 20 days old, our son had been under the knife more than some have in a lifetime, but we were confident his brilliant surgeon would perform. The hole in Jax's diaphragm was so large it required a Gore-Tex patch to close. His wound spanned his entire right side of his abdomen, but the job was done: Jax's liver and bowel were finally where they needed to be.
Initially, we were told should Jax survive, we needed to expect six to eight months in the NICU, at best.

While we knew it would be a huge shift in our lives, we were willing and ready to do whatever we needed, including moving to a new state to be with Jax. You can imagine our utter shock when, at only eight weeks old, Jax graduated from the NICU at the Children's Hospital of Philadelphia with a simple NG feeding tube. The medicines and oxygen, trach tube, and wiring we expected to have simply were not a part of Jax's story. We were stopped by no less than three doctors on our walk from the NICU to the car asking why and how we were leaving so soon. My husband and I rely heavily on science and are guided by the incredible medical field, but I will go to my grave knowing Jax is an absolute miracle.
Today, Jax is a thriving 2-year-old little boy.

Thanks to several months of post-hospital PT, OT, and speech therapy, Jax is developmentally up to speed with no feeding tube, oxygen, or medications. He absolutely blows his doctors away at every visit and continues to amaze anyone who comes in contact with him (especially if they've seen his medical chart). Jax loves sports and has a killer arm, is obsessed with animals, and absolutely adores his big sister. He is tough, hilarious, and a total snuggle bug. I've never met someone so ornery, yet so lovable. Jax insists on doing everything independently and truly keeps up with the best of them. He is tiny, but fierce, and has just recently noticed his (beautiful) scar and has started referring to it as his "strong boo-boo."
He is our miracle.

If there is one thing I want him to know, it's this: Jax, through all the uncertainty we've faced, there has always been one thing we've been so sure of and that is our love for you. We have known since we made our decision to fight for your life that every single day is going to be a roller-coaster, but we're willing to ride it for you. We need you to know no matter what happens, we are here for you. We want you to experience joy and excitement, love and wonder, disappointment and concern, fear, and uncertainty; we want you to feel it all and live each day with purpose. And I promise for every day you spent in the NICU, for every specialist appointment you have to attend, for every follow-up surgery, sickness, or struggle you face, we will make it up to you in love, hugs, kisses, and support. While your life may never be "normal," we promise to make it the absolute best it can be.
This story was republished with permission and was written by Kayte Ray. You can follow her journey on Instagram



