
Having options when it comes to birth control is key when you’re sexually active, especially if you’re not looking to conceive a baby at the moment. Depending on your lifestyle, health, budget and other preferences, the best birth control for you might not be the best for someone else — it’s not a one-choice-fits-all situation. That’s a good thing because choosing the best birth control for you gives you the power to plan your family and future the way you want.
We spoke with Dr. Tamika K. Cross, a board-certified OB-GYN, who leads the team at The Serenity Women’s Health & Med Spa team, along with Dr. Peace Nwegbo-Banks, also a board-certified OB-GYN. Located in Pearland, Texas, they give women the options they need to make proactive choices and plan their families on their own terms.
There are a lot of different factors to consider when choosing birth control.
Dr. Cross believes the most important factor to consider is if the patient has health concerns or medical problems. “One reason would be they can't have certain hormones, for instance,” says Dr. Cross. “Or if there's a history of hormone sensitivity or an allergy, especially an allergy to copper, then they can’t get ParaGard (a copper intrauterine device or IUD).”
When thinking about birth control, the patient should also consider what’s realistic for their lifestyle. “If they know they’re not going to reliably take a daily pill,” explains Dr. Cross, “then they should consider other options … But always talk to your doctor about those concerns and options to suit your needs. It's really just finding out what's best for that person.”
The side effects of the birth control you are considering is also a major factor to consider. For example, some common side effects of the birth control pill are nausea, headaches, weight gain, spotting, breast tenderness, and mood changes. Some women experience all of these side effects, some women only experience a few, and there are some women who experience none of these. As you’re going through the early stages of your birth control, you’ll notice similar changes — or not — and your doctor can help you adjust or try other birth control options.
There are so many different birth control options available today. Take your time deciding.

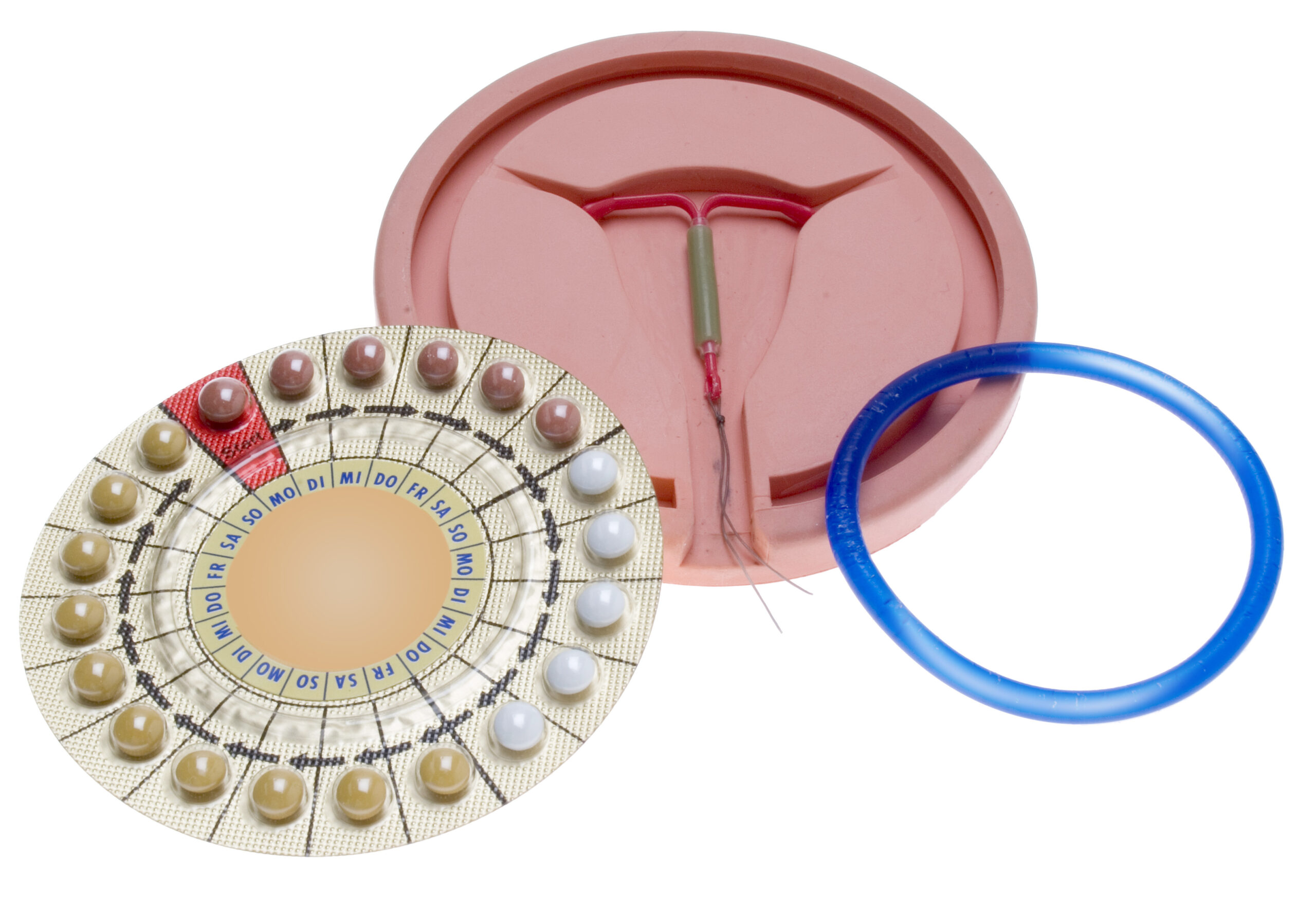
Short-acting hormonal birth control includes types of birth control that use estrogen or progestin hormones to prevent pregnancy. They work by stopping ovulation, thickening cervical mucus, or thinning the uterine lining, or a combination of all three.
Probably the most well-known form of short-acting hormonal birth control is the oral contraceptive, also called the birth control pill — or "the pill" — which is taken daily. Other options are the birth control patch, which is changed weekly, and the vaginal ring, which is worn for three weeks at a time. There is also a birth control injection which you would get every three months. “If they're going to get the shot,” Dr. Cross says, “you have to come in every three months and that just doesn’t work for everyone.”
For the above forms of birth control to be reliable in preventing pregnancy, they need to be implemented consistently. And please beware of mothers-in-law tampering with your birth control.
Long-acting birth control methods are, as expected, birth control methods that last for a longer amount of time than the short-acting types. Examples of the long-acting options are intrauterine devices — IUDs — and birth control implants that can last for three to 10 years. Most long-acting birth control options use hormones to prevent pregnancy — although a copper IUD is an alternative that doesn’t use hormones — and they generally don’t require any maintenance besides checkups during your annual wellness visit.
Dr. Cross says the class of birth control that she has seen an increase in her patients using is the LARC, long-acting reversible contraceptive. “I will definitely say in the last few years, the LARC,” she explains, “this is going to include your IUD and your Nexplanon, and the devices that we insert in the arm that can stay for up to three years that you don't have to think about every single day, like the pill.”
Long-acting reversible contraceptives are becoming more popular birth control for good reason.

“Research shows that the most effective birth control, technically, out of all those options are the LARC kinds,” says Dr. Cross. “But the highest one being the implant, the Nexplanon, the one that gets inserted in the arm, but then like 0.02% less than that is the IUD.”
So the LARC birth control options are all above 99% effective. That means they are just as effective as getting a tubal ligation (also called “having your tubes tied”), but Dr. Cross suggests that LARC options are “actually even more effective than getting your tubes tied” because LARC options are reversible. Having your tubes tied is a medical procedure for women who are sure they don’t want a future pregnancy.
If birth control that requires hormones or implants aren’t for you, there are the barrier methods.

Condoms, the sponge, cervical caps, spermicidal foam, and diaphragms are examples of birth control options that work by blocking sperm from entering the uterus, so these are used every time you have sex. They can be purchased at pharmacies, drugstores, and big box stores like Target and Walmart.
These options are usually the most economical choices for birth control (priced under $20). Other birth control methods are generally covered by most health insurance plans. Without insurance, birth control pills can cost an average of $35-$50 a month, and a birth control shot can range from $200 to $300 for the year. The cost of an IUD without insurance ranges from $500-$1,300.
Some people choose natural methods of birth control, such as menstrual cycle and ovulation tracking.

Natural methods of birth control are considered a lifestyle because they depend on the couple to be most responsible during sex. There’s the fertility awareness method where you keep an eye on your ovulation and the calendar, withdrawal (the pull out method, pretty self-explanatory), breastfeeding as birth control, and good ol' outercourse and abstinence are other natural ways of avoiding pregnancy. While these methods help avoid pregnancy, the chance of them not working is much higher. According to Planned Parenthood statistics, outercourse and abstinence are — as expected — 100% effective, breastfeeding as birth control is 98% effective (did you know that?!), fertility awareness is 76%-88% effective and the withdrawal method is 78% effective.
When it comes to male contraceptives, unfortunately their options are slim.

Obviously, condoms should definitely be on the table, because besides avoiding pregnancy, they protect you from sexually transmitted diseases, and that’s not true of any other method. But condoms are not a failsafe; they can break or otherwise be unreliable.
“In regard to condoms, I think they’re important to prevent STDs,” explains Dr. Cross, “but for birth control, the efficacy is like 80%, which is far from perfect. But now you're saying that there are birth control options that are 99% effective, why would I want the 80% option? It could break; it's like ‘oopsie, you're pregnant.’ OK, no, I think there should be a backup method.”
Should you use Plan B as birth control?

“No,” says Dr. Cross. “As you know, the trade name for the most popular one on the market is Plan B. And I hyper-focused on that name because it literally should be plan B. Because Plan A is having proper birth control. Plan B is supposed to be an alternative option afterwards. So this should not be used as birth control and is a high dose of hormone.” Dr. Cross reveals that when you look at “how many milligrams it is,” by taking a Plan B or Plan B-type pill you're taking what’s like “a whole pack of birth control all at one time, so there are going to be side effects with it. Avoid that scenario if you can.”
Once you’re ready to start trying to conceive, stop taking your birth control or see your doctor for removal if you have an IUD.

If you want to have a baby, generally, you can start trying to conceive whenever you feel ready after stopping birth control. Let your doctor know that you are trying. Many women find that they are able to get pregnant in anywhere from a month to a year of trying after stopping birth control, depending on individual factors.
Click here for more information about Dr. Tamika K. Cross and The Serenity Women’s Health & Med Spa.



